CALL US: 818.605.4082
Email US: surgeon1936@yahoo.com
Endovenous Thermal Ablation
Varicose vein, a disease of the superficial venous system, is characterized by a weakness of the vein wall causing vein distention/dilatation. Once distended /dilated, most valves, along the diseased vein, will become incompetent. This means: they will leak and the normal uphill - back to heart - blood flow, with the help of gravity, will reverse course and become a downhill flow, back to calf/ankle. This flow pattern is called reflux. That is the scenario only if the patient is upright on his/her feet. With patient recumbent, even better with elevated leg, the favorable gravitational forces, will automatically facilitate resumption of the normal uphill back-to-the-heart flow. (One can easily understand now the temporary, but beneficial effect of leg elevation.)
To make all this and the following sentences easier to understand, let's imagine an overflowing faucet. Obviously the escaped water, aided by (the same) gravity, in a free fall fashion, will be flooding the floor. Once leaking faucet is fixed and overflow properly controlled, future flooding should be prevented.
Truncal varicose veins (VV) present a very similar scenario. The "faucet"/escape point is, however, located either in the groin or behind the knee, places were leg’s superficial vein (called saphenous) will join deep veins (femoral in the groin; popliteal behind the knee), sites called junctions (SFJ respectively SPJ). These two junctions are normally protected by a major valve responsible not just for maintaining the normal back-to-the-heart, uphill flow but also to drain the blood from the superficial system into the deep. Therefore, as long as this valve is competent i.e. normal, in no circumstances blood, from the larger deep vein can spill into the superficial vein. Never! However, in the presence of a leaky i.e. incompetent junctional valve, blood from the deep vein, helped by gravity, (like the water in the presence of an overflowing faucet mentioned above), will escape into the superficial vein and will start its journey in an reversed, downhill fashion, flow pattern called reflux (Fig. 1).
Obviously, blood will not be “flooding" floors, but disease affected and already distended, bulging branches/tributaries of the vein that caused patient’s cosmetic distress in the first place. If, with passage of time venous pressure rises too, the patient may become symptomatic complaining of discomfort, pain, ankle swelling and complications such as superficial phlebitis, chronic venous insufficiency, venous ulcers may occur.
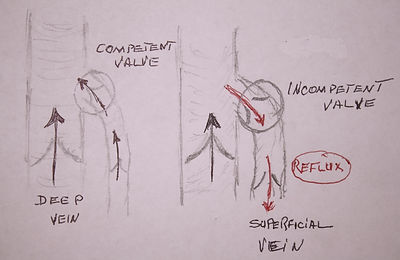
Fig. 1 Normal (uphill) and pathological (downhill) flow at the groin junction between the superficial long saphenous vein and femoral vein.

Truncal Varicose Veins:
Principals of care.
(Click to enlarge)
The main difference between the two scenarios is that water flooded the floor in a free fall fashion, while blood, in its downhill/reversed course, uses as a conduit, the existing axial superficial vein trunk extending from the groin junction to ankle (the long saphenous vein) or from behind the knee junction to the ankle (the short saphenous vein). This conduit, in normal physiologic conditions, collects uphill flowing blood through attached branches/tributaries existing along the entire leg. In varicose veins, as previously mentioned, flow is reversed i.e. downhill, from the axial vein into the branches/tributaries (Fig. 2). Positioned in slightly deeper structures of the thigh and calf, in most cases, this axial vein is not visible. (For more detailed information please read anatomy and physiology.)
To achieve the best therapeutic result, any treatment modality available for varicose veins has to follow three major steps. (See drawing).
Step 1. The method has to completely close/obliterate/stop the leakage of blood originating at the level of the escape point/junction regardless its position : groin or behind the knee.
Step 2. The method has to also stop (remove or close) the downhill pattern of blood flow existing in the saphenous vein trunk (either along the inner aspect of the thigh or along the hind side of the calf) being the axial conduit enabling the downhill/reversed pattern of flow ("reflux"), and permitting large volumes of blood to spill/”flood” the branches/tributaries of the axial vein, causing them further to distend/bulge.
Step 3. The method lastly, should also take care of the distended and bulging tributaries either removing or closing them, and if just possible, in the same session.
Endovenous thermal ablative procedures, meant to replace the need for the traumatic stripping surgery, use catheters/probes introduced under ultrasound guidance (through the skin) into the targeted main axial vein trunk. The procedure works only for straight vein trunks and not for the distended bulging tortuous branches. It is known for a long time that connective tissue, when heated, shrinks. This is the direct result from heat’s impact on collagen, a fibrous protein that makes up 90% of the organic material of all tissues, including veins. Collagen, is like a stretched out spring, but when heated the bonds, keeping the spring-like substance taut, are released shrinks into a jumbled coil shriveling tissue. The generated excessive heat is delivered slowly while the introduced probe is slowly pulled back and removed. The aim of the procedure is to close this straight main/axial vein trunk existing in the thigh or calf, and by this, interrupt/ablate the downhill flow of blood spilling into the bulging/distended varicosities (Step 2). Properly closing the proximal escape points/junctions (Step 1) is mandatory to secure long term results. However, using the endovascular ablative procedure, this is not properly possible . The escape point/junction, where the superficial vein trunk dead-ends in the deep vein (either in the groin or behind the knee), is easy to close/ligate only using the open/surgical approach but not with endovascular ablation for fear of a severe potentially lethal complications. To avoid this, the probe/catheter, is advanced up to 3-5 cm bellow the offending junction and basically leaving it open. Should the probe be fully inserted it could trigger blood clot formation, and blood clot at this level, could easily spill int0 the deep vein system, causing a deep vein thrombosis (DVT). If diagnosed, DVT may need a lengthy anticoagulation treatment and possible hospitalization. Moreover, should the clot dislodge and travel to the lungs it may end up causing pulmonary emboli (PE), a life threatening disaster. The left behind bulging varicose branches, (Step 3) not amenable to this method, will be removed with hooks or closed with sclerotherapy usually in a separate session(s) for obvious financial gains.
The reader is advised that due to the relative ease the procedure can be performed, as well as due to the offered financial gains, it could be abused. Patients with spider veins or insignificant size reticular even varicose veins should pay attention when submitted to an unnecessary duplex ultrasound examination that may discover an incompetent axial vein that "needs" to be closed. Have a second opinion as that axial vein trunk could be a life saver if needed, later in life, for a by-pass procedure. To prove my point I have recently participated in a local meeting organized by one of the most prestigious hospital in LA. A cardiologist, staff at the hospital and who in the last 3-4 years entered the venous field as well declared that in his patients with heart failure he is using the thermal ablation as this will improve the the heart failure. He never published his assumption as he now that it would never be published. I can only conclude that he is doing it for financial gains, for him personally as well as for the hospital.
There two main thermal options to choose from:
A. Endovenous radio-frequency (RF) ablation, ERFA or RFA formerly also known as VNUS or Closure, is using heat generated by a radio-frequency (RF) current/energy. RF currents have been used for long time during surgery for tissue cutting and coagulating small blood vessels in the operating field. Their wave length is between 3KHz -300GHz which are the wave lengths/frequencies of radio waves. For ablating a vein trunk the core temperature of the probe has to be 120º Celsius or 248 F but the temperatures on the vein wall is just below boiling point (180-190 F.) (Fig 3)
RF energy does not penetrate deep, does not cause pain but they can burn the skin, adjacent nerves, and can potentially induce blood clotting in the treated superficial vein. (See above) Today, besides closing veins there is a wide range medical use for RF current such as: in ablating tumors, in cardiology in case of arrhythmias, in pain management, sleep apnea, just to name a few.

Fig. 3 RF ablation catheter in action.
B. Endovenous laser ablation, EVLA or simply ELA (also known as EVLT) is using laser’s, (standing for Light Amplification by Stimulated Emission of Radiation), that are highly energized monochromatic light beams (as a form of electromagnetic radiation). Several wavelength/frequencies (measured in nanometers) are used by different companies: 810, 940, 1320 and 1470 meaning that none is perfect...Laser generated heat is targeting the red cells hemoglobin to generate hot steam that in turn will cause the needed injury besides to the same inner lining of the vein wall but also to the collagen existing in the vein’s wall.
Both endovenous methods are performed in an office setting using compartmental tumescent anesthesia – which is a form of local anesthesia - meant to also isolate the targeted vein from other close by structures (skin, nerves) and protect them from being "burned", which is not always guaranteed... Large volumes (up to 500cc and more) of mixed local anesthetic with saline, sodium bicarbonate and epinephrine are infiltrated around the targeted vein to distance and separate the superficial vein from the skin and a major nerve trunk. Should this nerve be injured/burned the patient will have sensation loss similar to that experienced after a dental anesthesia, only to last for a life time. While this method in my opinion is superior to foam sclerotherapy it has associated morbidity that can’t be neglected. Among them, the just mentioned skin burn and possible residual pigmentation, pain and induration/stiffness (due to heat perforation of the injured causing deep tissue collection of blood clot (hematoma) quite long time (weeks) needing continuous pain medication. All this point to a rough convalescence not existing with Ambulatory Phlebectomy. Thromboembolic complications have been mentioned in form of superficial phlebitis and deep vein thrombosis (DVT) caused by extension of clot from the treated superficial vein into the deep vein system (seen in 1-3 % of cases) making pulmonary emboli (PE) a dreaded possibility. Recently, a very sad case and outcome was presented to a group of physicians members of a professional organization I also belong . After an uneventful laser ablation procedure the patient after reached home, and after could not reach the practitioner, was taken to the emergency room because of a malignant heart arrhythmia. Tests have shown, that a segment of the laser probe's sheet broke loose and lodged in the right heart of the patient. Same night the patient underwent open heart surgery.!! This is my point, for a condition such as varicose veins, basically a cosmetic problem one should not offer and perform procedures that can risks the patient life. Risks should be taken and are taken only and only if we physicians have to intervene medically or surgically in real diseases that affect the quality of life or even endanger the life of a human being.
Immediate and late treatment failures in form of incomplete vein closure are frequently reported not to speak that the the cosmetic outcome could be unsatisfactory (Fig. 4) while ambulatory phlebotomy delivers constantly excellent cosmetic results and in much shorter time too! (Fig. 5).
I am pleased with my results - in 4000 plus cases with Ambulatory Phlebectomy - without any complication worth mentioning and excellent cosmesis. It is also performed in an office setting, local anesthesia and always, always in one single session. I had and have absolute no reasons to opt for the high-tech endovascular modalities that delivers a much inferior cosmetic outcome and also potentially exposes the patients to severe complications. I dully recognize I am in minority but I sleep well at night as I will never expose any of my patients to potentially severe complication. I consider varicose veins mainly a cosmetic problem and no patients in my vocabulary should - for basically a cosmetic condition - ever need to be hospitalized for a deep vein clot, put on anti-coagulation (blood thinning) therapy and /or followed for the possibility of a pulmonary emboli that can end in tragedy. Not in my vocabulary! Indeed the clever words of a former Roman slave Publilius Syrus "Some remedies are worse than the disease" resonates well with me!!
Fig. 4 Unsatisfactory results of thermal ablation (Picture from the net)


Fig. 5 The excellent cosmetic results with the minimally invasive Ambulatory Phlebectomy.
